Attio is the AI CRM for modern teams.
Connect your email and calendar, and Attio instantly builds your CRM. Every contact, every company, every conversation, all organized in one place.
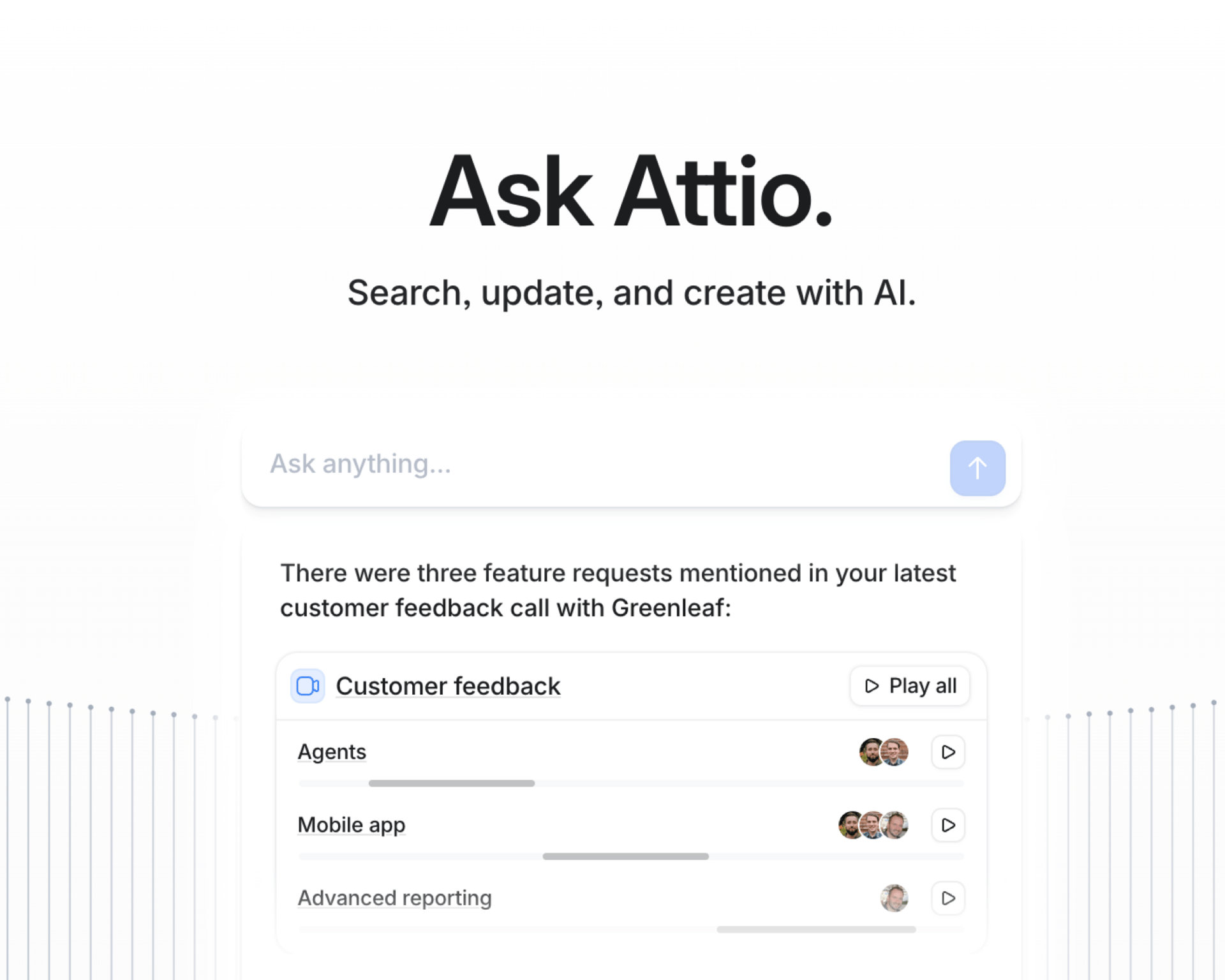
Then Ask Attio anything:
Prep for meetings in seconds with full context from across your business
Know what’s happening across your entire pipeline instantly
Spot deals going sideways before they do
No more digging and no more data entry. Just answers.
Welcome to the 6 new subscribers who have joined Future Human since our last edition! Join 366 other leaders learning about the future of human health by subscribing here:
Hi friend,
Welcome back to Future Human! I think I have mentioned a few times to you all that I am on my medicine clerkship here in NYC. The first of about 9 rotations this year in order to explore specialties and help me decide on my career path ahead. We are now 6 weeks into this 8 week block and things could not be going better. I have learned so much, spent so much time with patients, and witnessed incredible care delivered to those who need it most. Now that is all partially related to this newsletter, I also wanted to highlight the incredible technology I am seeing daily which advances the industry. I get pumped everyday with the things I see.
Just yesterday, we were debating what sneaky microbe could possibly be driving the infection picture of our patient after all our tests turned out negative. I quickly learned, for moments when you are stumped like that, there is now a company producing the Karius Test – a non-invasive, next-generation sequencing blood test that detects over 1,000 pathogens—bacteria, DNA viruses, fungi, and parasites—by identifying microbial cell-free DNA (cfDNA) in plasma. It is not cheap, but it can help you decide the proper antibiotic sooner by finally highlighting the bacteria, virus, fungus, or parasite at fault. Incredible! Hope to highlight them soon as a company when Workups return after I take my Step 1 board exam in March — those deep dive newsletters take time I currently do not have. Excited to write that up soon!
To more lives saved,
Andrew, Isabelle, and Nicholas

Andrew’s Take
Pharmacokinetics matter. What the body does to the drug — absorb, distribute, excrete — matters. Nowhere is that more true than in the brain. Understandably, the body makes it incredibly hard to get there because of the blood-brain barrier (BBB). Innovative teams have dedicated decades to try and cross it to treat different disease states. Dublin-based biotech Aerska just raised a $39 million Series A to do exactly that, aiming to get RNA medicines into the brain.
RNA-based therapies have already changed the game in a few diseases, but the brain has always been a fortress. The blood-brain barrier is great for keeping toxins out, but terrible for drug developers. Most large or complex molecules, including many RNA therapies, simply can’t get through in meaningful amounts.
Aerska’s bet is that delivery is the real bottleneck. The company is building what it calls a “brain shuttle” system — a way to systemically deliver RNA medicines across the blood-brain barrier without needing invasive procedures. Under the hood, this involves an antibody-oligo conjugate platform that’s designed to ferry genetic medicines straight to the brain, where they can actually do their job.
The new funding will help push this platform toward the clinic, with early programs focused on genetically driven neurological diseases, including forms of Alzheimer’s and other neurodegenerative conditions. That’s a big swing in a field where most treatments are still about managing symptoms.
What makes this especially interesting is that Aerska isn’t just pitching a single drug. They’re pulling the perfect platform approach. If they can make this work, it doesn’t just unlock one therapy — it potentially opens the door to an entire class of RNA treatments for the brain. This round is a bet that the future of neurology might be less about better pills and more about finally getting the right molecules to the right place.

Andrew’s Take
I have been in med school for only 18 months. In that short time, I have already been pulled onto two projects applying AI to cardiac imagery to extract valuable data. Many teams across countless institutions have the same idea. Mayo Clinic researchers showed recently that AI can estimate a patient’s ejection fraction — the key number cardiologists use to measure how well the heart is pumping — using only a single still image from an echocardiogram (a classic ultrasound of the heart we order constantly) instead of a full video.
Traditionally, calculating left ventricular ejection fraction has required watching the heart beat in motion and manually measuring changes in chamber size. Not too complex, but time consuming. The new approach uses computer vision to infer that dynamic information from one snapshot, which could make it much easier to use in busy clinical settings. If we could get our echo results sooner, wow, I’d be able to explain to my attending why the pro-BNP came back at 30,000 pg/mL!
In Mayo’s study, the team trained a convolutional neural network on thousands of echocardiogram frames and tested it across multiple Mayo sites and handheld ultrasound data. The model performed very well overall at classifying ejection fraction, especially when the estimate was averaged across more than one independent frame, and across both standard and point-of-care imaging.
Aside from my desire to get immediate results and un-delay my gratification, there are many other benefits. Reducing the amount of data needed could lower computational costs and accelerate assessments in clinics, emergency departments, or rural settings where imaging resources are limited. The researchers note that more work is needed to test the model across diverse patient populations and real-world point-of-care scenarios, but this proof of concept points toward a promising future.

Andrew’s Take
When I first read that Hims & Hers was not giving up on the GLP-1 profit stream, I had a suspicion that Novo would step in ASAP to stop them. I think I refreshed the browser twice before the next headline said they were being sued. Called it! Novo Nordisk is suing Hims & Hers over cheaper, unapproved versions of its blockbuster weight-loss and obesity drugs. Novo is accusing Hims & Hers of patent infringement by marketing compounded copies of semaglutide-based treatments like Wegovy and Ozempic outside the typical FDA approval process. This has been a point of tension for months, but the new release of their oral Wegovy copycat brought the battle back into the spotlight.
Hims & Hers announced plans to sell its own compounded version of the newly approved oral Wegovy pill at a significantly lower price point. That move drew swift backlash from not only Novo Nordisk, but also regulators. The FDA and Department of Health and Human Services jumped right in to pressure them against it as they aim to crack down on compounded GLP-1 products that haven’t gone through formal review for safety or efficacy. Facing this scrutiny, Hims & Hers backed away from its launch of the $49/month pill, but Novo Nordisk’s lawsuit now covers both the pill plans and the injectable compounded products that Hims has sold for some time.
Novo Nordisk argues that allowing widespread sale of these knockoffs threatens patient safety, undermines intellectual property protections, and erodes the regulatory framework that governs drug approvals. Hims & Hers, for its part, has pushed back, characterizing the suit as an attempt to restrict consumer choice and affordability in the weight-loss drug market.
This case highlights growing tension between traditional pharma companies and digital health platforms trying to leverage compounding loopholes to make popular therapies more accessible. The loophole I speak of allows pharmacies to create customized versions of approved drugs for individual patients without going through full FDA approval, sometimes letting companies sell unapproved copies. The outcome of this suit could influence how personalized and compounded medications are regulated and sold in the future.

Andrew’s Take
We have ad supported everything — Netflix, ChatGPT, and now healthcare. An ambitious plan, but now backed by quite the sum of money. Lotus Health AI just closed a $35 million Series A round to scale a pretty ambitious idea: free, AI-powered primary care for everyone. The funding is aimed at building out the product, hiring more clinicians, and expanding access while keeping the service free to users.
Lotus is trying to rethink the front door of healthcare. Instead of waiting weeks for an appointment and paying copays, patients can hop on a 24/7 AI-driven system that collects symptoms, reviews medical history, and pulls together relevant data in minutes. The company’s pitch is that software can handle much of the busywork that slows primary care down, letting clinicians oversee far more patients than in a traditional clinic model. Not the most shocking idea, but the business model is wild. Lotus doesn’t charge patients or bill insurance. Instead, it plans to make money through sponsorships inside the app. That’s a bold move in healthcare, and whether it’s sustainable is still an open question. But the bet is clear: if you can make primary care truly free and frictionless, you might get people in earlier, manage problems sooner, and save money across the system.
Under the hood, it’s not just a chatbot handing out advice. The AI handles intake and drafts a care plan using medical records, labs, wearables, and clinical guidelines, but board-certified physicians review and sign off on diagnoses, prescriptions, and referrals before anything goes to the patient. It’s a “doctor in the loop” setup designed to keep things safe while still moving fast. I am a sucker for any unconventional idea, no matter how outlandish. At the very least, it’s a fresh take on a part of healthcare that badly needs new ideas.

Andrew’s Take
Many names are taking on AI drug discovery. In the last year, what you may recognize if you follow the biotech/pharma space is that few are developing an asset in isolation. Like the pharma companies they are partnering with, these companies are building platform products that can be licensed by any user rather than accepting the risk of their own singular asset. Iambic Therapeutics, for example, just secured a $1.7B investment from Japanese pharma company, Takeda. The partnership is designed to accelerate the hunt for new medicines by combining Takeda’s deep disease expertise with Iambic’s AI platforms, which are built to model complex biological systems and propose novel therapeutic ideas faster than traditional methods.
Under the agreement, Takeda will fund multiple discovery programs over the next several years, with a focus on areas that have historically been tough for conventional drug research. Iambic’s technology uses machine learning to explore vast chemical and biological possibilities, prioritize promising targets, and generate outright new molecular ideas. Not to beat a dead horse, but if this works out it could cut down the time and cost it takes to move from concept to a potential drug candidate (getting tired of repeating that line I cannot lie)
For Takeda, this move reflects a broader industry shift toward leaning on AI not just for data analysis, but as an active partner in inventing new therapies. Instead of the conventional trial‑and‑error approach, the idea is that AI can uncover patterns and opportunities that human researchers might overlook, especially in complex diseases. For Iambic, the deal brings not only capital but validation from a top global pharma player. That backing could help the startup scale its platform and attract talent, while giving Takeda a front‑row seat to emerging AI‑driven drug concepts.
This falls in perfect line with the growing trend where big pharma companies are outsourcing some of its early discovery work to nimble, tech‑centric companies. Whether it is buying high speed biotechs with early assets or partnering with AI platform teams, they are trying to move faster while managing risk. If successful, these collaborations could reshape how new medicines are found and de‑risked long before clinical trials begin.
We hope you enjoyed this edition of Vitals!
We always appreciate feedback, questions, and conversation, so feel free to reach out on LinkedIn or by replying to this email.
To more lives saved,,
Andrew, Nicholas, and Isabelle